Researchers recently evaluated the function of renalase (RNLS) as an independent predictor of coronavirus disease 2019 (COVID-19)-related mortality and released their findings to the Research Square* preprint server.The immunological response to the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has been the focus of several biomarker investigations over the past few months, which have also raised important new questions. Those who have deadly symptoms are said to have pathophysiology that can be separated from people who experience milder symptoms by an aggressively disrupted inflammatory response. Renal damage is among the signs that have changed, but these alterations seem to be transient.
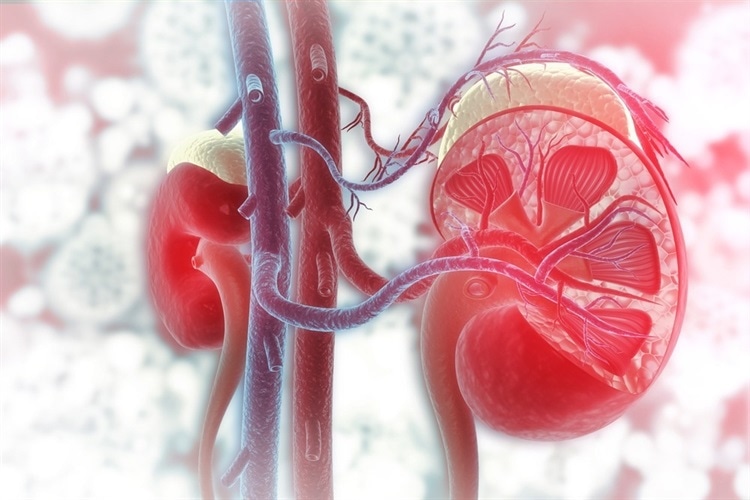
The dynamic behavior of these indicators and the decreased markers in SARS-CoV-2 infection are poorly understood. Renalase, an endogenous peptide produced by the heart, kidney, and endothelium, exhibits prosurvival properties, including the ability to prevent the production of cytokines in viral infections like COVID-19 in mouse models.Researchers examined if renalase may independently predict COVID-19-related mortality in the current investigation.
The team looked into adult patients who tested positive for COVID-19 and were hospitalized in a city academic hospital between March 1 and June 30, 2020. All patients had severe SARS-CoV-2 infection, as determined by nasopharyngeal swab samples and reverse transcription-polymerase chain reaction (RT-PCR). All imaging and specimen collection were done in accordance with accepted medical practices.
In order to obtain clinical data from the electronic medical record system, the team used the Department of Medicine COVID Explorer (DOM-CovX), a group of hospitalized COVID-19 patients. This information included sociodemographics, vital signs, comorbidities, laboratory measurements, disposition, and procedures throughout the entire hospital stay.
The admission date, symptoms with onset dates, smoking history, immunocompromised state, cardiopulmonary resuscitation, as well as dates of death, intubation, and last completed follow-up, were extracted using manual chart reviews. The cohort’s serum or plasma specimens were analyzed as follows by assessing inflammatory markers, including interferon (IFN)-ɑ, IFN-β, IFN-λ, IFN-Ɣ, interleukin (IL)-1β, IL-6, and tumor necrosis factor (TNF), along with kidney injury molecule (KIM-1).