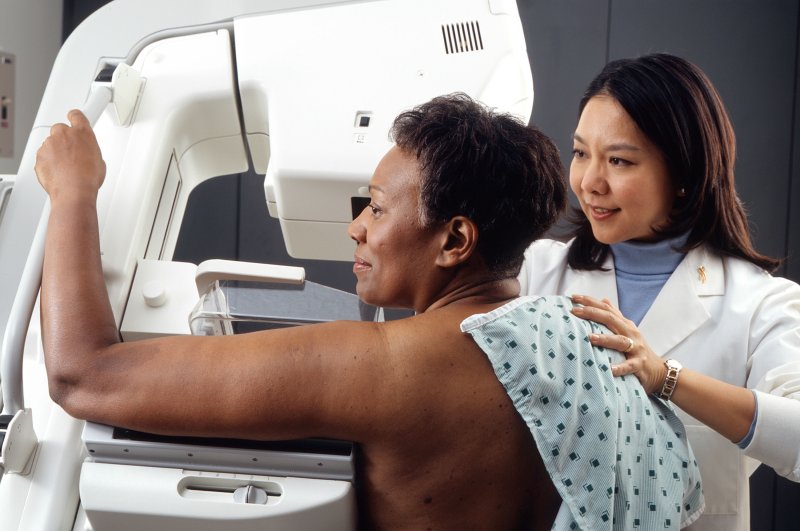
According to new federal standards, mammography centers must inform women if they have thick breasts and provide a description of how the tissue appears on the X-ray.
On a mammography, it may be more challenging to find cancer in dense breast tissue. Breast cancer risk is also increased by having thick breasts.
The Mammography Quality Standards Act (MQSA) of 1992’s standards are amended by the U.S. Food and Drug Administration (MQSA).
Chief Medical Officer Dr. Hilary Marston said, “Today’s move exemplifies the agency’s broader commitment to promote innovation to prevent, detect, and treat cancer.Since 1992, the FDA has worked to ensure that patients have access to high-quality mammography, she said in an FDA news statement. “The Mammography Quality Standards Act has had a substantial impact on public health, including a sharp decline in the number of facilities that don’t adhere to quality requirements. As a result, more women will have access to reliable, high-quality mammography. We are still dedicated to strengthening the fight against breast cancer and pushing initiatives to promote women’s health.”
The upgrade also makes it easier for doctors to classify and rate mammograms and increases the FDA’s control over and enforcement of facilities.
The initial statute was created to guarantee high-quality mammography, a crucial technique for detecting breast cancer early on.The modifications contain precise language describing how breast density may impact mammography accuracy. They advise women who have thick breasts to discuss their own situation and the chances of developing cancer with their doctor.
A complete breast health approach, according to the FDA, includes encouraging patient access to information on the effect that breast density and other variables can have on breast cancer risk.The amendments must be implemented within 18 months, FDA said.
They will enhance the agency’s ability to communicate directly with patients and healthcare providers when a facility is not meeting quality standards and is failing to communicate adequately with patients about that.
The goal is full communication of important information that could affect patient care decisions, such as the need for more screening.
Over a lifetime, about 1 in 8 women will get breast cancer, according to the U.S. Centers for Disease Control and Prevention. Mammograms continue to be the best tool for breast cancer screening and detection, the FDA noted.